Abstract
Background: Malnutrition is an important factor in patients for allogeneic hematopoietic stem cell transplantation (allo-HCT). Valid and convenient methods are required for determining muscularity to evaluate severity of malnutrition, and a secondary analysis of computed tomography (CT) images is an accessible method for this evaluation. Compared with several CT-based methods for sarcopenia (degenerative muscle loss), the impact of the prognostic value of sarcopenia in patients with acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) following allo-HCT remains controversial.
Patients and Methods: We retrospectively reviewed the data of 125 adult patients with AML and MDS who had undergone allo-HCT for the first time between 2000 and 2016. Sarcopenia was assessed using the following CT-based evaluation methods at the time of transplant: skeletal muscle index (SMI) and mean muscle attenuation (MA) at third lumbar vertebrae (L3) level. SMI (cm2/m2) was calculated using the cross-sectional imaging area of the following skeletal muscles (cm2): rectus abdominus, abdominal (lateral and oblique), psoas, and paraspinal (quadratus lumborum and erector spinae) muscles and was normalized by height. The CT Hounsfield unit (HU) thresholds were −29.0-150 for skeletal muscles. Mean MA HU was calculated for the fatty tissue infiltration of the muscles at L3 level using previously reported HU thresholds. Sex-specific cutoffs for both SMI and MA were determined using ROC analysis. Threshold values of SMI and MA, demarcating significantly lower survival at 100 days from allo-HCT, were defined as sarcopenia. Fifty-two (41.6%) patients were defined as having sarcopenia on the basis of muscle mass and the fatty infiltration of muscle. In the patients with sarcopenia (n = 52) and those without sarcopenia (n = 73), SMI values (mean ± SD) were 45.6 ± 4.2 and 52.4 ± 5.1 cm2/m2, respectively (P < 0.001), and MA values (mean ± SD) were 33.6 ± 1.7 and 35.4 ± 1.6, respectively (P=0.021). We evaluated correlation between the sarcopenia and prognosis in patients with AML and MDS following allo-HCT.
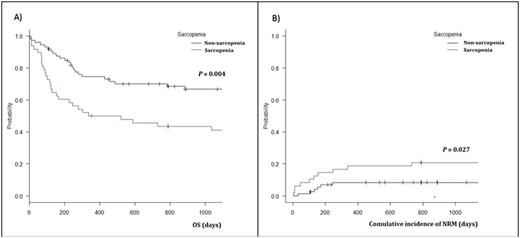
Results: This study enrolled 125 patients, including 73 males and 52 females, with a median age of 47 years (16-65 years) at transplant. Body weight, serum total protein, body mass index (BMI), SMA, and skeletal MA were significantly higher in the males than in the females. There were no significant differences in the sex, age, Eastern Cooperative Oncology Group performance status, and other characteristics of the patients at allo-HCT. A median follow-up was 1198 days (8-5230 days).In the patients with sarcopenia and those without sarcopenia, at 2 years of overall survival was 43.5% and 70.1% (95% CI, 0.293-0.569 and 0.579-0.794, respectively; P= 0.004, Figure 1), respectively; disease-free survival was 52.9% and 68.6% (95% CI, 0.324-0.619 and 0.558-0.784, respectively; P= 0.031), respectively; cumulative incidence of relapse was 37.5% and 21.5% (95% CI, 0.239-0.511 and 0.127-318, respectively; P= 0.239), respectively; and non-relapse mortality (NRM) was 20.8% and 8.4% (95% CI, 0.106-0.334 and 0.034-0.164,respectively; P= 0.027, Figure 1). Causes of NRM were as follows: infection in 10 patients, TMA in 2 patients, acute GVHD in 6 patients, chronic GVHD in 3 patients, cerebral bleeding in 2 patients, and unknown causes in 2 patients. Infection was the major cause of NRM in patients with sarcopenia (7/11 deaths as NRM from infections). The patients with sarcopenia showed a longer duration of hospitalization than those without sarcopenia, in terms of the median number of days from transplantation to discharge (88 and 74 days, respectively; P= 0.026). Univariate and multivariate analyses revealed that sarcopenia is a prognostic predictor of NRM (HR, 2.24; 95% CI, 1.41-4.81; P= 0.031).
Conclusion: The results of this study suggest that among 125 patients with AML and MDS who had undergone allo-HCT for the first time, the presence of sarcopenia was associated with a lower survival rate and higher NRM, resulting in longer duration of hospitalization.
Fujisawa: Bristol-Myers squibb: Honoraria; Chugai Pharmaceutical: Honoraria; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.